Cervical cancer symptoms: Signs, screening and prevention
Published February 2023 | 4 min read
Expert contributors Professor Marion Saville, executive director of the Australian Centre for the Prevention of Cervical Cancer; Associate Professor Megan Smith, co-leader of the cervical cancer and HPV stream at the Daffodil Centre
Words by Angela Tufvesson
Thanks to screening and an effective vaccine, cervical cancer is one of the most preventable cancers. New developments bring us closer to the goal of elimination.
Cervical cancer is one of the most preventable cancers, with experts believing it could be eradicated globally as early as 80 years from now, thanks to the cervical cancer vaccine and regular cervical cancer screening. These help to protect against the virus that causes the disease, and pick up pre-cancerous changes.
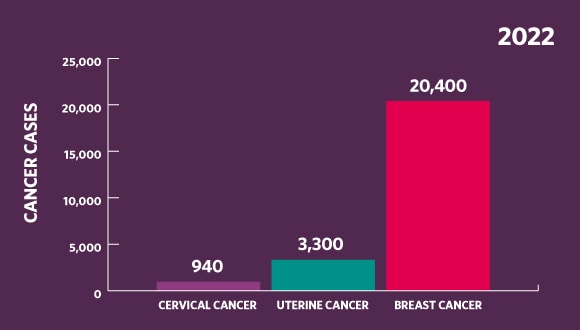
Source of all statistics: canceraustralia.gov.au/affected-cancer/cancer-types
In 2020, the World Health Organization set a target to work towards eliminating the disease in every country by reducing cases to below four per 100,000 women. Australia is currently on track to get there by 2030. In 2022, 940 Australian women were diagnosed with new cases of cervical cancer – well below the 20,400 women who received a breast cancer diagnosis and the 3,300 women who learned they had uterine cancer. But that’s still 940 women too many.
“The goal is to eliminate cervical cancer as a public health problem by the end of the century globally,” says Professor Marion Saville, executive director of the Australian Centre for the Prevention of Cervical Cancer.
Keeping up to date with screening and getting vaccinated are the best ways to protect yourself and your family from cervical cancer – and contribute to this milestone global goal.

What causes cervical cancer?
Cervical cancer happens when abnormal cells grow in the lining of the cervix. What makes it different from other cancers is almost all cases are caused by a common sexually transmitted infection called ‘human papillomavirus’ (HPV).
“That is the key difference between cervical cancer and pretty much every other cancer,” explains Associate Professor Megan Smith, co-leader of the cervical cancer and HPV stream at the Daffodil Centre, a research centre for cancer control and policy.
The other main risk factor for cervical cancer is smoking.
Assoc Prof Smith says cervical cancer rates halved in Australia in the decade after the introduction of the cervical cancer screening program in 1991 and have remained “relatively low” ever since. Further developments in screening and the introduction of the HPV vaccine may help cervical cancer rates to decline even further.
“Because Australia is off to such a great start, our modelling has suggested that we could actually get below that World Health Organization threshold [of four per 100,000 women] relatively soon, probably around 2030,” Assoc Prof Smith says.
If cervical cancer is not prevented, treatment can be effective when the disease is found early, according to the Cancer Council, and most women can be treated. “Early detection can still lead to really good outcomes because early-stage disease is very treatable,” says Prof Saville.
Cervical cancer symptoms
HPV and precancerous changes in cervical cells usually show no symptoms.
The average age for diagnosis of cervical cancer is 47 years, and 70% of this type of cancer is diagnosed in women under the age of 60. The most common symptoms, according to Cancer Council Australia, include:
- vaginal bleeding between periods
- menstrual bleeding that’s heavier or longer than usual
- vaginal bleeding after menopause
- pain during sex or bleeding after sex
- pelvic pain
- changes in vaginal discharge like a strong or unusual colour or smell.
Prof Saville says even though these symptoms can be signs of other less serious conditions, it’s important to get them checked out.
”For any abnormal bleeding, always go to your doctor and ask about it – even if you had a negative screening test yesterday,” she says. “Screening is something we do for people without symptoms. Anyone with symptoms should see their GP.”
Cervical cancer screening
Because cervical cancer is almost always caused by HPV, screening for the virus does two important things: it enables early detection of any abnormalities and acts as a preventive measure.
“The goal of cervical screening is to pick up things at a pre-cancerous stage that can be treated more easily,” says Assoc Prof Smith. “It can be a matter of removing a small amount of tissue through surgery rather than, for example, doing a hysterectomy, which would often be required for cervical cancer treatment.
“Most people who get cervical cancer have either never been screened or are overdue.”
In 2017, a new test that checks for HPV called the cervical screening test replaced the Pap test, which tested for changes in cervical cells. This means women only need a test every five years.
“Screening is very, very effective,” says Assoc Prof Smith. “It will dramatically reduce your risk, particularly now that we've got the new test, which is much more sensitive.”
Even better, because the new HPV test checks for the virus, there’s no need to collect cells from the cervix, Assoc Prof Smith explains. “The upshot of that is you can use a swab to collect cells from your vagina and do the HPV test on that.”
From July 2022, women became able to choose whether to self-collect their own sample using a swab, or have it collected in the usual way by a GP.
Unlike the bowel cancer screening program, Prof Saville says a self-collected cervical cancer screening still “takes place within the context of a trusted relationship” with a GP – it's done under the supervision of a healthcare professional. “You're given a swab to collect it at the end of the consultation, either behind a curtain or in the bathroom.”
Assoc Prof Smith says this is a major development that can address equity in Australia and help make elimination of cervical cancer a reality. Rates of cervical cancer among Aboriginal and Torres Strait Islander women, for example, are as high as 20 per 100,000, compared to seven per 100,000 for non-Aboriginal and non-Torres Strait Islander women.
“We haven't been able to get screening to everybody in Australia – there's a lot of inequities,” she says. “This option for self-collection should be a lot more flexible and hopefully improve that.”

Cervical cancer vaccine
Vaccination is the other key to elimination. The HPV vaccine protects against seven types of HPV, which cause around 90% of cervical cancers in women and around 90% of other HPV-related cancers in women and men. It also protects against two non-cancerous types, which cause 90% of genital warts.
Australia was the first country to introduce an HPV vaccination program for girls (age 12 to 13) in 2007, and one of the only countries to extend it to boys (age 12 to 13) in 2013, which Assoc Prof Smith says helps to create a ‘herd effect’. The vaccine was also developed in Australia by 2006 Australian of the Year Professor Ian Frazer and his colleague, Dr Jian Zhou.
“There’s indirect protection that a lot of other people get because we've vaccinated so many people in the population,” she says. “It's a very, very effective vaccine.”
In February 2023, the Australian government changed the HPV vaccine schedule from two injections to one injection. This change comes from the Australian Technical Advisory Group on Immunisation’s (ATAGI) advice, who have considered the latest international scientific and clinical evidence. The data shows a single HPV vaccine dose gives comparable protection to healthy young people
This same evidence may prompt the World Health Organization to switch to a single-dose recommendation more broadly, which Prof Saville says makes it “much more possible to expand the reach of vaccination across the world”.
Young people (except those who are immunocompromised) who receive a single dose before 26 years of age are now considered fully vaccinated and don’t need further doses.
Do you have questions?
Chat to your GP about any abnormal symptoms or risk factors you may have or if you have any questions or concerns. An in-person visit is always best but if you can’t get to the GP practice, you can chat to a doctor using a telehealth service like GP2U where you can have an online consultation from the privacy of your own home or wherever you can access the internet.
Our partnership with GP2U, an online video GP service, makes it easier for you to access telehealth services.
Through our partnership with GP2U, all HCF members with health cover can access a standard online video GP consultation (up to 10 minutes) for a fee of $50. See hcf.com.au/gp2u for more information.
RELATED ARTICLES
Treating breast cancer
Breast cancer treatment has come a long way in recent years, with Australian women now receiving a more targeted and personalised approach.
STIs: what you need to know
It's a health issue we don’t talk about enough. If you’re sexually active, get the facts.
Bowel cancer prevention
One in 12 Australians will develop bowel cancer. Knowing the signs, and regular screening are key to tackling the disease.
Health checks by age
Your guide to staying on top of your health with the right screening checks for every life stage and age.